Abstract
Background: The association of mutations in genes related to hereditary anemias (HA) can affect disease phenotype and severity. Understanding HA genetic basis is crucial for avoiding misdiagnosis and for adequate clinical management. β-thalassemias (BT) are characterized by a reduction of β-globulin production caused mainly by point mutations within the HBB gene or its bordering sequences. The imbalance between α and β globin production results in ineffective erythropoiesis and hemolysis. Hereditary spherocytosis (HS) is characterized by abnormalities of erythrocyte membrane proteins, resulting in spheroidal, osmotically fragile erythrocytes with varying degrees of hemolysis and anemia. HS related to spectrin deficiency is clinically heterogeneous, ranging from well-compensated hemolysis to severe anemia. Here we describe two unrelated cases in which patients had a chronic severe hypochromic microcytic hemolytic anemia with elevated HbA2 clinically compatible with BT Intermedia or Major. However, conventional β-globin gene sequencing revealed only BT trait that did not justify the clinical presentation. The extensive research for deletions or other mutations for BT were negative. We then proceeded with additional genetic investigation through exome sequencing.
Aims: To investigate additional mutations related to HA that may contribute to a phenotype of severe anemia in patients with a β -Thalassemia trait.
Methods: Patients' clinical features and laboratory results were collected by medical charts evaluation. The Institutional Review Board approved this research and patients signed written informed consent. β-globin gene sequencing was initially performed by conventional Sanger sequencing. Exome sequencing was performed utilizing the Illumina HiSeq2500 platform.
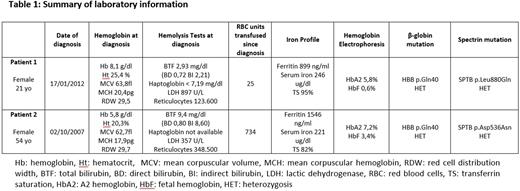
Results: Patient 1 had a clinical picture of eventual transfusion dependence, moderate hepatic iron overload and splenomegaly. Peripheral blood smears showed hypochromic microcytic red blood cells, together with spherocytes and circulating erythroblasts. Her father was asymptomatic, with a mild hypochromic microcytic hyperproliferative anemia, and her mother had normal hemoglobin and reticulocyte counts. Patient 2 had a clinical presentation of transfusion dependence, extramedullary paravertebral hematopoiesis, moderate hepatic iron overload, mild pulmonary hypertension and leg ulcers. Peripheral blood smears showed hypochromic microcytic red blood cells, together with a moderate number of spherocytes and circulating erythroblasts; clinical and laboratory data from her relatives were not available. Laboratory workup is shown in Table 1. Exome sequencing was performed and, beyond the previously known β-globin mutations, mutations in spectrin gene were found in patient 1 (SPTB p.Leu880Gln) and patient 2 (SPTB p.Asp536Asn). The father of the Patient 1 was diagnosed with a heterozygous mutation in HBB gene, while her mother was diagnosed with a heterozygous SPTB p.Leu880Gln mutation, which did not result in anemia nor in significant hemolysis. Both spectrin mutations were already described in the literature: SPTB p.Leu880Gln was reported in association with a mutation in SPTA1 gene, resulting in a moderate anemia, while SPTB p.Asp536Asn mutation was described in an non-anemic individual.
Conclusion: Our results indicate that the association of heterozygous BT and spectrin mutations may result in a phenotype of moderate to severe anemia. These data show that, in unusual severe cases of presumed BT trait, mutations responsible for HS should be investigated.
Disclosures
Fertrin:Agios Pharmaceuticals: Consultancy, Membership on an entity's Board of Directors or advisory committees, Research Funding, Speakers Bureau; Sanofi Genzyme: Consultancy; Global Blood Therapeutics: Consultancy, Speakers Bureau. Costa:Global Blood Therapeutics: Membership on an entity's Board of Directors or advisory committees; Novartis: Honoraria; Global Survey HCP Steering Committee for Global Blood Therapeutics (GBT): Consultancy.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal